- Diabetes
Insulin
Insulin prescriptions available online
Manage your type 1 or type 2 diabetes with insulin. Book an appointment with one of our board-certified doctors online. Get a new prescription for insulin or refill an existing insulin prescription today.*
Book an appointmentTreats diabetes, type 1 and 2
Fast-acting, intermediate, and long-acting options
Manages blood sugar levels effectively
*Prescriptions are provided at the doctor’s discretion. Learn more about our controlled substances policy and how you can save up to 80% with our prescription discount card.

About insulin
Insulin is a term that refers to medications designed to regulate the amount of glucose (sugar) in the blood. They’re often used to help treat type 1 (T1DM) and type 2 diabetes (T2DM), but they’re also used for other conditions. There are 3 main types of prescription insulin.
Insulin is a hormone made by the beta cells in your pancreas. It takes glucose from carbohydrates consumed and converts it to the energy that your body uses right away or stores for later use.
It helps stabilize your blood sugar levels and keeps them from going too low (hypoglycemia) or too high (hyperglycemia).
Even though your body needs sugar for energy, the sugar usually can’t get into your cells directly. You need this pancreatic hormone released from your pancreas and signal cells to soak up the sugar from your bloodstream. This process allows the sugar to enter your cells and be used for energy.
If your body makes more sugar than it needs, this hormone will signal it to be stored in your liver and released it when your blood sugar levels get too low. In other words, it helps your body balance your blood sugar levels and keeps them within normal range.
If your body can’t produce enough of this hormone, cells become resistant to how it should normally work, you can develop hyperglycemia. This can cause complications like diabetes if your blood sugar levels stay too high for too long.
What insulin treats
The most common condition treated with human insulin is diabetes. The drugs are designed to replace or supplement the body’s natural hormones.
These medicines allow blood glucose to enter cells and enable the body to store blood sugar more adequately for later use. This helps address a significant problem in people with diabetes mellitus: high blood sugar.
Other conditions are also treated with this therapy. Mild-to-moderate diabetic ketoacidosis, for example, may need management with this approach. Learn more about this and other off-label uses of this therapy below.
Diabetic ketoacidosis
Diabetic ketoacidosis is a serious and potentially life-threatening complication of diabetes. It is most common in people with T1DM, but people with T2DM can also develop it. Diabetic ketoacidosis occurs when the body doesn’t have sufficient amounts of insulin to encourage blood sugar into the cells for use as energy.
The injections can reverse ketoacidosis and are essential for successfully managing this complication. In this case, the hormone promotes glucose use by peripheral tissues, suppresses ketogenesis, and diminishes glycogenolysis and gluconeogenesis.
Gestational diabetes mellitus
Gestational diabetes mellitus (GDM) is a condition wherein a hormone made by the placenta prevents the body from using insulin properly. It develops during pregnancy. Instead of being absorbed by the cells, glucose accumulates in the blood.
What makes GDM different than T1DM is that it’s not the lack of the hormone that causes the problem but other hormones that decrease its effectiveness. Some, but not all, pregnant women need human insulin to treat GDM. The role of this therapy is to lower blood sugar levels.
Hyperosmolar hyperglycemic state
Hyperosmolar hyperglycemic state affects people with T2DM whose blood sugar levels are severe or abnormally high (sometimes over 40mmol/l). This state may develop over a few weeks or result from other problems, such as dehydration. It requires emergency medical service, i.e., immediate help.
This therapy can help with the mild-to-moderate hyperosmolar hyperglycemic state. The first line of treatment in the emergency room is aggressive fluid management, after which a patient receives an insulin drip once the blood sugar levels fall below 50mg/dl/hr.
How insulin works
It functions by making the body move sugar from the bloodstream into the cells. The cells use blood sugar for energy i.e., fuel for the body. In people with T1DM, the pancreas doesn’t produce this hormone at all.
However, in people with type 2 diabetes, the body doesn’t produce sufficient amounts of the hormone or can’t use the produced amounts properly. This often happens due to insulin resistance, a common problem in people with type 2 diabetes.
Regardless of the underlying cause, a lack of this hormone forces glucose to remain in the bloodstream. Hyperglycemia, high blood sugar, ensues. The injections copy or mimic the body’s own in response to food. It is similar to the hormone the pancreas produces naturally. Extra levels of the hormone improve the management of blood sugar and reduce the risk of diabetes complications.
Side effects of insulin
When taken as recommended, analog insulins are generally well tolerated. However, they can still cause some side effects.
The more common side effects of insulin include:Swelling of arms and legs
Hypoglycemia (low blood sugar)
Weight gain
Injection site reactions (redness, itching, swelling)
Lipodystrophy (skin changes at the injection point)
Anxiety or depression
In rare cases, insulin may cause serious side effects. These can include:
Severe hypoglycemia
Hypokalemia (low blood potassium)
Serious allergic reaction
Swelling of hands and feet
Heart failure
Eye complications
Insulin risks
These therapies are generally safe, but there are some risks if you have other medical conditions or take certain prescription pills.
Before you take prescription insulin, be sure to tell your healthcare provider if you have any of the following conditions or issues:Liver disease
Kidney disease
Thyroid problems
Excessive alcohol consumption and alcoholism
Adrenal/pituitary gland problems
Insulin drug interactions
When you begin a new medication, tell your healthcare provider about any other medicaments, supplements, or herbs you take. Some medications that might interact with this therapy include:
Other antidiabetic agents, such as thiazolidinediones
Anti-hypertensive medicaments
Pills for heart rate disorders
Medications that treat cholesterol
Pain relievers
Blood thinners
Corticosteroids and sympathomimetic agents (for allergy or asthma)
Protease inhibitors (for treatment of HIV infections)
Some antibiotics
Therapies for tuberculosis
Medicaments for psychiatric disorders
Beta-blockers and other medicaments for heart disorders
Insulin FAQs
How should I take insulin?
Because you can't take the therapy orally, it must be injected with a syringe, pump, or insulin pen.
The type of injection method you get prescription for will depend on your personal preference, your health status, and the type of insurance you have.
Before you start taking the therapy, your healthcare provider or a diabetes educator will teach you how to administer the injection on yourself or a loved one. You'll also learn how much insulin you need.
Parts of the body that you can inject include:Upper arm
Abdomen
Thigh
Buttocks
Some people only need to inject themselves once a day. Others will need to inject themselves several times a day and take other diabetes medication such as Metformin. Your healthcare provider will work with you to determine the right amount (units) of insulin required and whether you need rapid-acting, long-acting, or both. Most people need two up to three vials per month for optimal diabetes care. You can change the site location of your injection each time in order to prevent thickening of your skin, bruising or local infection.
Be careful not to inject it within two inches of your belly button. Your body won’t absorb it as well at this location.Who shouldn’t take insulin?
People with low blood sugar, liver problems, decreased kidney function, and low amounts of potassium in the blood shouldn’t take this therapy. If you have these health problems, make sure to inform a healthcare provider about them. They will determine whether it’s safe to take and buy insulin and make the best recommendation for your condition.
How long does it take for insulin to work?
The answer to this question depends on the type of therapy. For instance, rapid-acting insulins start working within 15 to 30 minutes after the injection, and its effects peak within 60 minutes while their length lasts two to four hours.
On the flip side, regular- or short-acting insulins takes 30 minutes to work but its effects last longer around three to six hours. The effects peak within two to three hours, however.
When it comes to intermediate-acting insulins, it takes around four hours to work, the effects peak in four to 12 hours whereas the duration is 12 to 18 hours. Long-acting insulins starts working within two hours and its duration is 24 hours, while ultra-long type starts working within six hours and its effects last 36 hours or longer.
Buy insulin your trusted healthcare provider recommends.What should I avoid with insulin?
When taking this therapy you should avoid injecting it in the same exact place every time. Doing so could lead to lipodystrophy, the breakdown of fat under the skin, or the formation of lumps and indentations that obstruct the absorption of this hormone. For that reason, it is necessary to rotate injection sites, as many insulin manufacturers advise.
Additionally, avoid injecting it too deeply. Otherwise, it could enter the muscle, and the body could absorb it too quickly. Avoid waiting more than 15 minutes to eat after taking mealtime therapy.
Also, you should avoid an unhealthy diet, especially refined carbs. And most importantly, it is necessary to avoid taking it with certain medications to avoid interactions. It may interact with other antidiabetics, antidepressants, anti-hypertensive medications, some pain relievers, therapies for cholesterol, somatostatin analogs, protease inhibitors, some antibiotics, and others.
If you’re taking medications with which this therapy interacts, make sure to inform the healthcare provider beforehand.What does insulin do to blood sugar?
This hormone helps blood sugar enter the cells, which then use it for energy. Plus, it sends a signal to the liver to store blood sugar for later use. When a person injects it, it helps move blood sugar out of the bloodstream into the cells. The cells use a portion of that sugar for energy, while the remainder is stored in the liver, muscles, and fat. As blood sugar moves to cells, its levels should return to normal.
Is insulin the same as sugar?
It is not the same as sugar. Blood glucose (sugar) is the main sugar in your body. Insulin is a peptide hormone produced by beta cells of pancreatic islets. The main function of this hormone is to regulate blood sugar. Since both play an important role in diabetes, it’s easy to assume they’re the same. However, they are different things with entirely different functions.
Does insulin require a prescription?
Like other medications for the management of this lifelong condition, it usually requires a prescription. In some cases, patients can get it over the counter, but this is rare. While insulin prices have increased over the years and vary based on the insurance coverage, you can enroll in savings program specifically created to help people get therapy they need with cost savings. You can also connect with diabetes community to share experiences and learn more about different prices, pharmacies, and even get useful tips for better quality of life.
How is insulin prescribed?
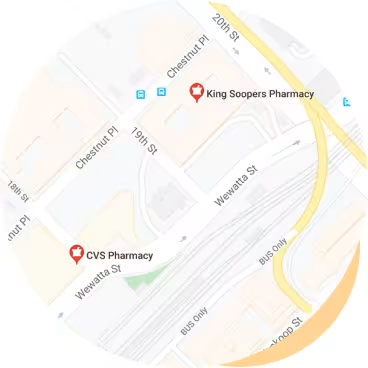
A healthcare provider issues a prescription to a patient with T1DM or T2DM. Besides standard appointments at a doctor’s office in a hospital or clinic, patients can also access doctors from websites and online platforms. This makes the whole process a lot faster and you can buy insulin easier, especially for patients with a busy lifestyles. The only thing necessary is to pick up your monthly supply at retail pharmacies close to you.
What is the most common insulin prescribed?
Healthcare providers usually recommend basal therapy, i.e., intermediate-acting and/or long-acting forms. The greatest advantage of these types of insulins is that they help regulate blood sugar levels throughout the day. The most common insulins in terms of strength in the United States are U-100, i.e., 100 units of the hormone per milliliter of fluid, according to the American Diabetes Association.
Are there other ways of injecting yourself beside a syringe?
Yes. You can use an insulin pen. They usually have a cartridge filled with solution that you can insert into the pen and discard after all the medication has been used. The dose that you need can be dialed on the pen. The solution is injected through a needle, like a syringe.
Another method of administration is through an insulin pump. These pumps help you manage your complicated condition by giving you this hormone 24 hours a day. This is done through a catheter which is placed under your skin. The pump allows you to control the number of hormones your body gets.How do you monitor yourself when taking insulin?
This therapy is a must for people with T1DM. It may also be used for people who have T2DM whose blood sugar levels aren’t well-controlled by medication alone.
If you get diagnosed with diabetes, a healthcare team will help you create an insulin program that will help keep your blood sugar levels normal, along with setting you up with a healthy diet and exercise plan.
Many people with diabetes usually start out by taking two injections per day and gradually go up to three or four injections per day. They may take one or two types of insulin, depending on their blood sugar levels throughout the day.
Keeping track of your blood sugar levels over time can help you understand how exercise, stress, or different types of food can affect your levels. You can use this data to predict how your body will react to the therapy and you will have a better chance of avoiding episodes of hyperglycemia (high sugar levels) or hypoglycemia (low blood sugar levels).
There are a few factors that can affect how your blood sugar levels fluctuate, including:When and how much you exercise
The type of foods you eat
The injection site
Time of day and frequency of injections
Stress
Illness
3 simple steps to getting insulin online

Step 1
Book an appointment to discuss insulin.
Book a same day appointment from anywhere.

Step 2
Talk to your doctor online.
See a doctor on your smartphone or computer.
Step 3
Pick up your insulin prescription from your online doctor.
We can send prescriptions to any local pharmacy.
Insulin pricing details
How pricing works
To get insulin online, join our monthly membership and get discounted visits.
Paying with insurance
Membership
$16.99/month
First month free
Visits
Copay
30 days of free membership
Same-day appointments 7 days a week
Unlimited messages with your Care Team
Prescription discount card to save up to 80%
Exclusive discounts on lab tests
Free memberships for your family
Cancel anytime
Visit price with insurance
Often the same as an office visit. Most patients with in-network insurance pay $30 or less!
We accept these insurance plans and many more:
Paying without insurance
Membership
$16.99/month
First month free
Visits
$129
30 days of free membership
Same-day appointments 7 days a week
Unlimited messages with your Care Team
Prescription discount card to save up to 80%
Exclusive discounts on lab tests
Free memberships for your family
Cancel anytime
Visit price without insurance
Initial visits are $129.
If we're unable to treat you, we'll provide a full refund.
Insulin resources
Sources:
PlushCare is dedicated to providing you with accurate and trustworthy health information.
Lilly Insulin Lispro. Homepage. Accessed on October 16, 2023 at https://www.lillyinsulinlispro.com/.
American Diabetes Association. Insulin Basics. Accessed on October 16, 2023 at https://diabetes.org/health-wellness/medication/insulin-basics.
Mayo Clinic. Diabetes Treatment: Using Insulin to Manage Blood Sugar. Accessed on October 16, 2023 at https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-treatment/art-20044084.
Centers for Disease Control and Prevention (CDC). Types of Insulin for People with Type 1 Diabetes. Accessed on October 16, 2023 at https://www.cdc.gov/diabetes/basics/type-1-types-of-insulin.html.
PlushCare content is reviewed by MDs, PhDs, NPs, nutritionists, and other healthcare professionals. Learn more about our editorial standards and meet the medical team. The PlushCare site or any linked materials are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment.